My Protocols: Dosing Myself AND Others with Rapamycin.
Learn how to safely use and monitor this Longevity Drug
On LinkedIN today it is revealed by Krister Kauppi that I am taking Rapamycin with good effect. Most doctors don’t like to share their medical histories or their medicine or supplement use. Since Krister is mentioning my outcomes with Rapamycin I figured it is time for my readers to understand why I use this medicine and what I hope to gain from it. But first, my history. I was a collegiate (albeit brief) swimmer before I discovered “socializing” in college. So for every 10,000 yd practice I managed to have less salubrious activity. Unfortunately and fortunately this all stopped in medical school as there is no time for those shenanigans.
So with a body like that I bet I would live forever. Except, my family history betrays me. As a geneticist I must not over count the importance or lack of importance of my genome and epigenome. My mother died from a blood clot in her 60s, my father died of metastatic renal cancer in his 60s. It already sounds ugly. So in order to give myself the best shot I decided to add Rapamycin to my longevity stack. ONLY AFTER writing it since 2014 for patients in my practice and since using it since 2008 as an immunosuppressant for children at Mount Sinai. Yes, I have been helping patients with Longevity for over a decade and nearly have 2 decades experience with this medicine as a physician…. and during that time I have seen the highs and the lows of using this medicine off label. So, today I want to share with you the my protocols for this. If you want to skip the history lesson, just skip down to the bottom. But for those who are interested in how this medicine began it’s use as a Longevity Drug, read below. And for those who just want the facts, there is a version below the story, just for you. What follows after that is how I use this medicine for patients and myself.
From Easter Island to the Edge of Immortality: The Story of Rapamycin
In the early 1960s, a small team of Canadian researchers stepped off a military plane and onto the ancient soil of Easter Island. Their mission wasn’t to uncover lost Moai statues or decode Polynesian petroglyphs. They were collecting dirt. Specifically, they were hunting for exotic soil microbes that might harbor new antibiotics.
Buried in that volcanic earth was a microbe called Streptomyces hygroscopicus—a humble-looking bacterium with a remarkable secret. When they brought it back to the lab, the scientists discovered it secreted a compound with powerful antifungal properties. They named it rapamycin, in honor of the island’s native name, Rapa Nui.
At first, rapamycin looked like just another addition to the antibiotic shelf—interesting, but not revolutionary. That all changed when researchers noticed something peculiar: rapamycin didn’t just stop fungus. It halted cell growth. All cell growth. It was cytostatic, meaning it paused cells mid-division. That made it a candidate for cancer research. But more immediately, it found its first practical application in a very different field: organ transplantation.
By the 1990s, rapamycin had become a vital immunosuppressant. It helped prevent rejection in kidney transplant patients by tempering the immune system, and in 1999, the FDA gave it the green light. It was useful. Reliable. But still, it was boxed in—categorized as a niche drug for a very specific population.
And then came the twist.
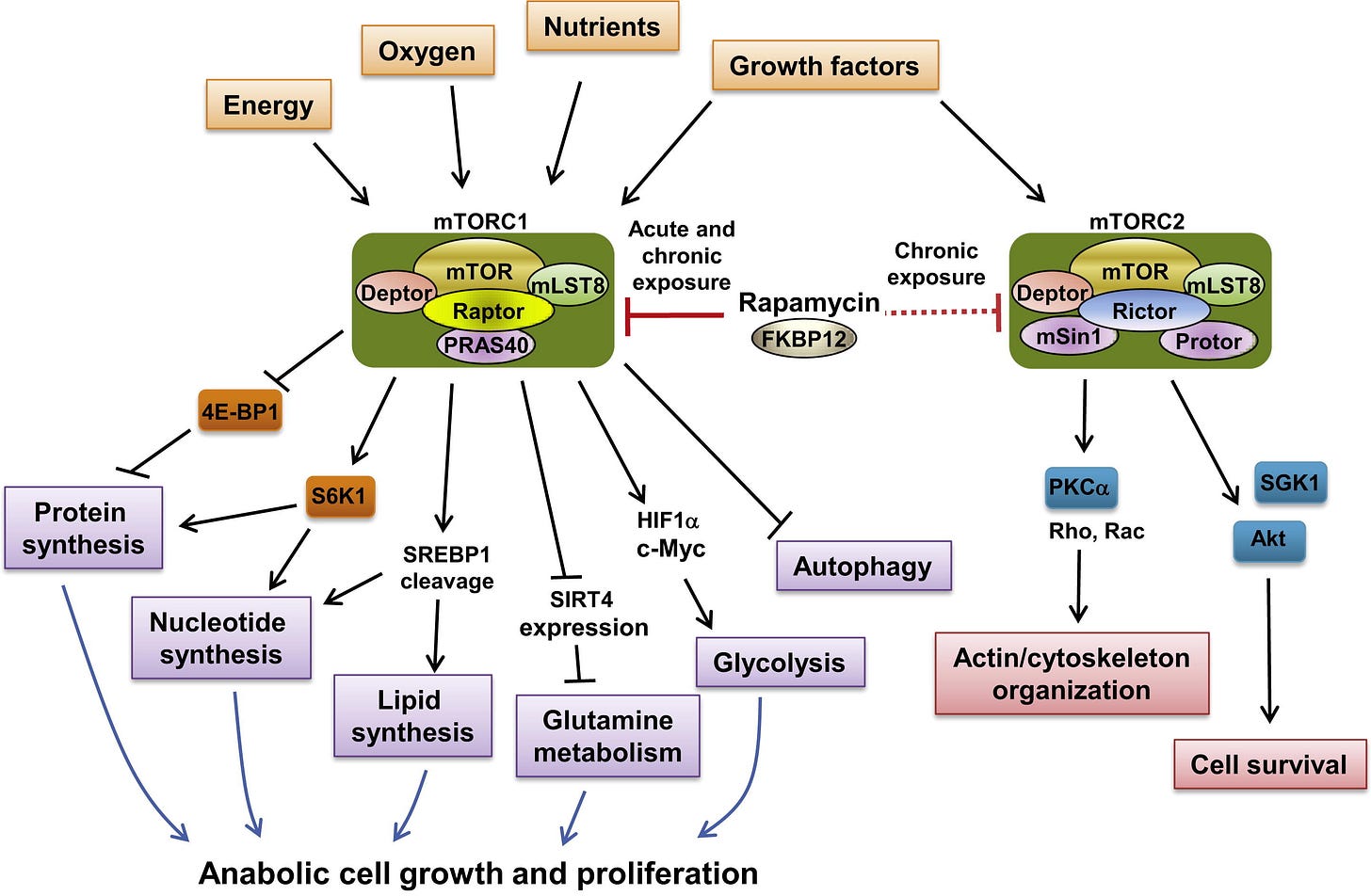
In the 2000s, a growing wave of longevity scientists started to take a second look at rapamycin. The compound’s mechanism—its ability to inhibit a protein complex known as mTOR (mechanistic Target of Rapamycin)—wasn’t just relevant to immune cells. It turned out mTOR played a central role in regulating aging itself.
mTOR is like the metabolic traffic cop of the cell, deciding when to grow, when to store, when to clean up. When it’s overactive—as it often is with age—it accelerates cellular damage, inflammation, and disease. Rapamycin slows that clock. In lab animals, it didn’t just delay disease—it extended lifespan. Not by days. By double-digit percentages. Even when given late in life.
In a 2009 study that stunned the scientific world, researchers at the Jackson Laboratory gave rapamycin to mice equivalent in age to 60-year-old humans. The result? The mice lived longer and healthier lives. It was the first time a pharmaceutical had shown such dramatic effects on aging in a mammal. And it kicked off a quiet revolution.
Since then, rapamycin has become the longevity community’s worst-kept secret. Used off-label by a growing number of physicians, it is prescribed in low, intermittent doses—enough to nudge mTOR into rest mode without suppressing the immune system. Patients taking rapamycin under supervision often report sharper thinking, reduced inflammation, better biomarkers, and even cosmetic improvements like tighter skin. Anecdotal? Perhaps. But the data keeps accumulating.
So how does a transplant drug end up in the medicine cabinets of biohackers, CEOs, and age-defying physicians? Because rapamycin is, in many ways, the first true anti-aging drug.
It doesn't just mask symptoms. It targets a root cause. And unlike trendier molecules that come and go with TikTok cycles, rapamycin has decades of clinical use, safety data, and a mechanism tied directly to the biology of aging.
Of course, it’s not a magic pill. It’s not risk-free. It requires intelligent dosing, medical oversight, and an understanding of timing, cycles, and trade-offs. Too much rapamycin and you may suppress your immune system. Too little and you might not get the benefits. Like all good medicines, it’s a tool—powerful in the right hands, dangerous in the wrong ones.
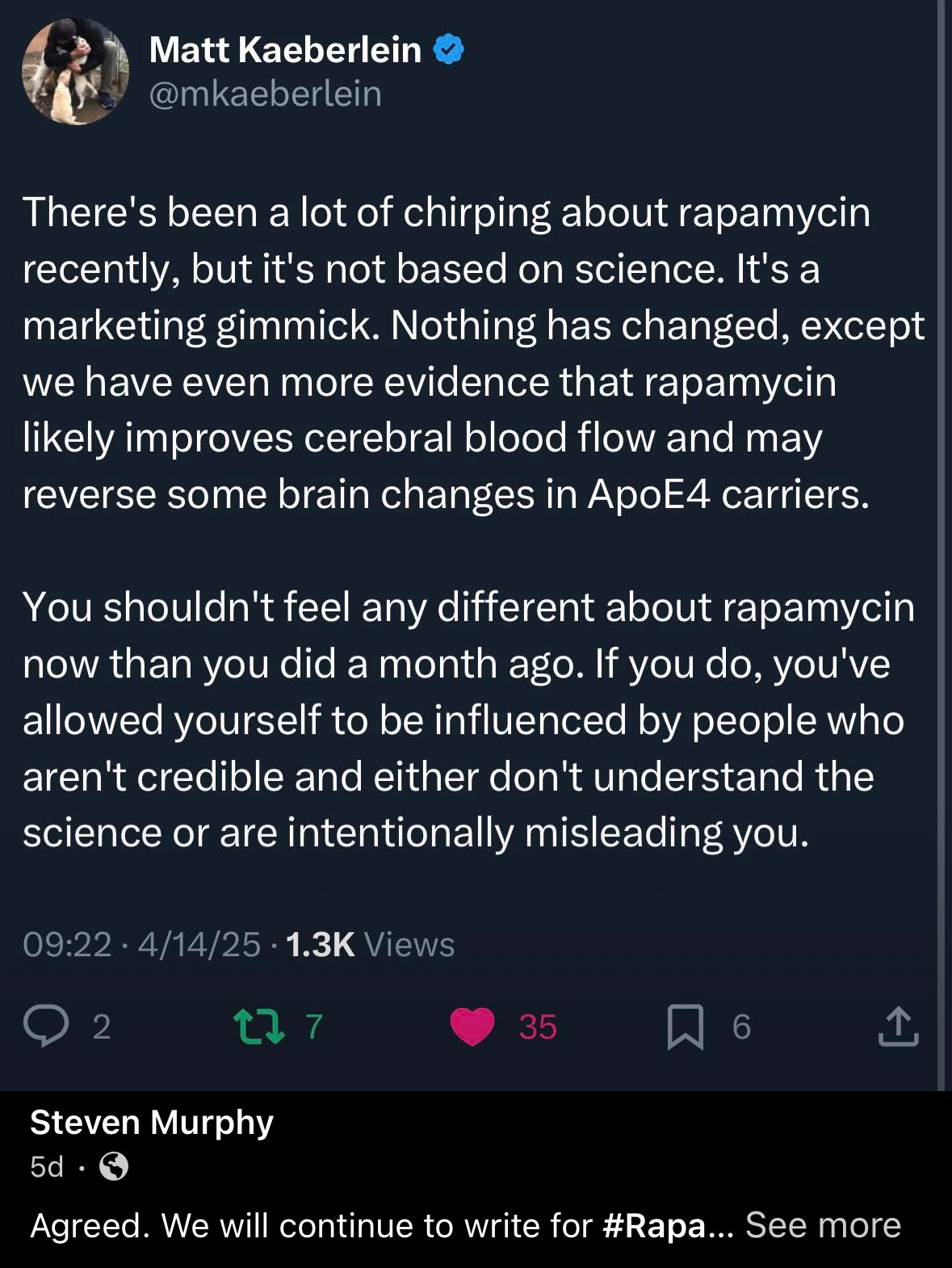
Today, new analogs of rapamycin are in development. Trials like the PEARL study are exploring its potential in healthy older adults. Companies are patenting slow-release formulations. And yet, the pure, generic version of this once-forgotten soil compound continues to draw attention for one reason: it works.
From a patch of dirt on a remote Pacific island to the forefront of anti-aging science, rapamycin’s journey is far from over. In many ways, it’s just beginning. And as we enter an era where medicine is no longer about treating disease, but reversing the biology of aging, rapamycin may prove to be the molecule that changed how we think about time—not just as something to endure, but something we can finally manage.
Rapamycin and Longevity: A Pharmacological History and Evidence-Based Review
For those who just want the facts…..
Rapamycin, also known as sirolimus, was first discovered in 1972 from a bacterium (Streptomyces hygroscopicus) found in the soil of Easter Island, also known as Rapa Nui. Originally investigated for its antifungal properties, it soon became apparent that rapamycin possessed powerful immunosuppressive and anti-proliferative effects. These attributes led to its FDA approval in 1999 for use in preventing organ transplant rejection. However, the story of rapamycin did not end with transplantation medicine—it evolved into one of the most compelling compounds in the field of aging and longevity research.
At the core of rapamycin’s effect is its inhibition of a protein complex called mTOR (mechanistic Target of Rapamycin), a critical regulator of cell growth, protein synthesis, metabolism, and autophagy. Rapamycin specifically inhibits mTORC1, the nutrient-sensing arm of the mTOR pathway, which is known to be overactive in many aging-related processes. By dampening mTORC1 activity, rapamycin helps restore cellular recycling, reduce inflammation, and preserve stem cell function. These effects address several of the biological hallmarks of aging and contribute to its role as a potential longevity-enhancing therapy.
The strongest evidence supporting rapamycin’s role in longevity comes from animal studies. In a landmark 2009 study published in Nature, researchers showed that administering rapamycin to middle-aged mice (equivalent to about 60 human years) extended their lifespan by 14 percent in females and 9 percent in males. These findings were striking because the intervention was initiated late in life and still yielded substantial lifespan extension. Additional studies confirmed that rapamycin-treated mice exhibited improvements in immune function, cardiac health, cognitive performance, and a delay in the onset of various age-related diseases, including cancer. Researchers also noted that intermittent dosing preserved these benefits while minimizing risks associated with chronic exposure.
In human studies, the data are still emerging, but early trials are promising. A 2014 study published in Science Translational Medicine by Mannick and colleagues found that low-dose everolimus (a rapamycin analog) enhanced the immune response to influenza vaccination in older adults, suggesting potential for reversing immune aging. While no long-term lifespan trials have been completed in humans, several ongoing studies, such as the PEARL trial, are evaluating rapamycin's safety and effectiveness in healthy aging populations.
Clinically, rapamycin is gaining traction among longevity-focused physicians who prescribe it in intermittent, low-dose regimens once weekly or divided doses three times per week. This approach minimizes side effects such as mouth ulcers, elevated lipids, and insulin resistance, which are more common with daily or high-dose use in transplant settings. When used intermittently, rapamycin appears to preserve mTORC2 function, which is critical for metabolic health and insulin sensitivity.
The potential downsides of rapamycin include immunosuppression, especially at higher doses or in patients with comorbid conditions. However, in healthy individuals monitored regularly, these risks appear to be minimal. Physicians often co-prescribe metformin to mitigate any effects on glucose metabolism and encourage a lifestyle that includes exercise, omega-3 supplementation, and regular lab monitoring of lipids, insulin, and blood counts.
In short rapamycin is arguably the most studied and validated pharmacological agent for lifespan extension in mammals. Its mechanism directly targets the mTOR pathway, a well-established regulator of aging. Supported by decades of preclinical data and growing human evidence, rapamycin is emerging as a foundational component of science-based longevity medicine. With appropriate patient selection, monitoring, and clinical oversight, it offers a promising avenue for those seeking to proactively address the biology of aging and prevent chronic disease.
If you are interested in using this medicine for your patients or for yourself keep reading below. In this part of the post I give you an informed consent, a dosing regimen and protocol that you can adopt for your P&T board or for your team .
Keep reading with a 7-day free trial
Subscribe to Longevity Insider with Dr. Murphy to keep reading this post and get 7 days of free access to the full post archives.